Prof. Javad Parvizi, Director of the Fellowship Programme at The Rothman Institute in Philadelphia on the right of this photo in theatres

Prof. Chitranjan Ranawat and Dr. Amar Ranawat, at The Hospital for Special Surgery in New York in their office
I would like to take the opportunity first to thank the BOA and Zimmer for funding my travelling fellowship to the USA.
Having undertaken an MD at University College London on management of periprosthetic joint infections (PJIs) after hip and knee replacements, I wanted to visit leading centres in the world to further enhance my knowledge of new strategies to combat PJIs and hence my choice of Hospital for Special Surgery (HSS) and The Rothman Institute. I have indeed spent 5 great weeks with Dr Amar Ranawat at HSS and Professor Javad Parvizi at The Rothmans Institute where I have learnt alot about PJIs and lower limb arthroplasty primary and revision procedures. At both centres, there are clear protocols for prevention and treatment of PJIs with regular active research into new strategies to improve PJI management.
Research on PJIs has proven that prevention is the most effective way of managing PJIs and hence the robust mechanisms of prevention being strictly implemented at both centres starting with the assessment and appropriate selection of the right patient to undergo an operation then optimising the patient and surrounding environment to achieve the best results.
A great amount of work has been led by Professor Parvizi and his team on diagnosing PJIs with the latest being the introduction of synovial fluid biomarkers such as human α-defensin 1-3, neutrophil elastase 2, bactericidal/permeability-increasing protein, neutrophil gelatinase-associated lipocalin, and lactoferrin, which correctly predicted the Musculoskeletal Infection Society (MSIS) classification of all 95 patients included in a recent study, with 100% sensitivity and specificity for the diagnosis of PJI. It was a huge privilege for me to observe how those tests are performed under the appropriate indications and utilisation of the tests to appropriately diagnose PJIs.
Managing established infections also follows clearly defined protocols with overall high rates of controlling PJIs at both centres. Among the interesting themes I have been exposed to and felt are important in managing PJIs are the implementation of the MSIS definition of PJIs, the multi-disciplinary approach to treating PJIs, patient medical optimisation peri-operatively, pre-operative diabetic control, pre-operative skin preparation, the operating room environment and controversial preventive strategies, antibiotic prophylaxis, workup of patients with suspected urinary tract infections, bone cement and antibiotics, diagnosis of PJIs in inflammatory conditions and culture negative PJIs, management of atypical PJIs and fungal infections, the role of irrigation and debridement and one and two stage exchange arthroplasty in managing PJIs. Furthermore, I have learnt alot about revision arthroplasty procedures in terms of implants used and indications for various procedures performed. I have observed a number of direct anterior approaches (DAAs) to the hip which are commonly used at The Rothman Institute for hip replacements, femoral osteoplasties and periacetabular osteotomies. Interestingly, the surgeons performing DAAs there do not use a Hana or Arch table whilst doing the procedure which gave me the opportunity to learn
how such a procedure can be performed freehand. I have also observed how to perform a Hardinge approach in a supine position which is the method of choice for performing lateral approaches to the hip at The Rothman Institute. I have been impressed with the perioperative pain management protocol implemented by Dr Ranawat which allows patients’ discharge at 2 and 3 days postoperatively following hip and knee replacements respectively. Additionally, I learnt his approach to soft tissue releases whilst performing knee replacements and using anatomic reference points to achieve soft tissue balance both in hip and knee replacements.
This fellowship not only improved my knowledge of managing PJIs but also introduced me to the differences between the healthcare systems in the USA and the UK. For example, as the healthcare system is private in the USA, the attending physician is bound to see all patients with the fellows in the clinics and is required to be scrubbed in any critical step of an operation even if the fellow or a senior resident is capable of doing the procedure independently. Additionally, there is a well-established role for physician assistants (PAs) in the USA with a clear pathway for studying this as an independent specialty and then for PAs to take up essential roles such as providing inpatient care on wards alongside residents, seeing patients in clinics similar to fellows and being the first assistants in the operating room. I have to say that I have been impressed with how well PAs function in different teams and how much their contribution improves overall efficiency. Likewise, operating room technicians are well versed with all instruments used for various procedures and most of the time function as first assistants in any operation which aids in a high turnover of patients and effective utilisation of theatre time.
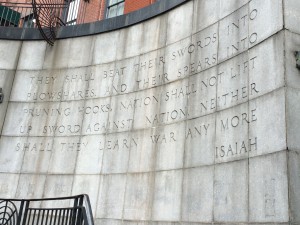
Similar to university hospitals in the UK, there are dedicated teams working on research and I had the great pleasure of involving myself with a number of research projects and publications during my visit to both centres. Last but not least, I have enjoyed the sightseeing in New York and Philadelphia having visited most of the tourist attractions in both cities.
Overall, this has been a unique experience for me and again I would like to thank BOA, Zimmer, Dr Ranawat and Professor Parvizi for giving me the opportunity to visit HSS and The Rothman Institute.